
Health Care & Wellness
Rural Health Transformation Program 101 (Federal Grants to States to Improve Rural Healthcare)
December 18, 2025 | Brock Ingmire
February 21, 2025 | Brock Ingmire

Key Takeaways:
Despite prescription drug costs controlling the headlines on how state legislatures are attempting to address rising health care costs, the affordability of provider services is an increasing priority for state lawmakers. Provider services are any type of care rendered by a health care professional, including doctors, nurses, therapists, or facilities. In 2024 and looking ahead to 2025, key issues that state lawmakers will continue to examine in order to limit the growth of health care provider costs include:
Certificate of Need (CON): Standards and review criteria utilized by states to either approve or prohibit major capital expenditures and projects by health care entities (i.e., new facilities or services).
Facility Fees: Fees that are often billed by hospitals or other similarly situated facilities with the intent to compensate for operational expenses of maintaining the facility and are distinct from a provider fee.
Surprise Billing: An unexpected medical bill that requests the patient to pay for the difference between the amount their health insurance pays and the full cost of a service, particularly when a provider is not in the patient’s insurer’s network.
Billing and Cost Transparency: Efforts that require health care providers and insurers to disclose certain information about the costs of items and services rendered to consumers.
State lawmakers are utilizing these levers to lower health care costs for consumers by attempting to increase market competition by providers, incentivizing providers to render care in appropriate settings for the level of care needed, and making insurers cover as much of the cost for services rendered as possible. In 2024 alone, 21 states used one or two of these levers to enact significant reform, and it’s likely other states will follow their lead in 2025.
Confronted with the fact that medical costs are expected to have increased between 7 and 7.5 percent by the end of 2024, and have the potential to increase between 7.5 and 8 percent in 2025, state lawmakers have felt compelled to respond. There are a few trends from legislation enacted in 2024, including:
Expediting Certificates of Need (CON): Creating expediting review and approval of certain CON applications and establishing exemptions from the CON requirements for certain services and facilities (i.e., psychiatric facilities most commonly).
Prohibiting Certain Facility Fees: Prohibiting providers from charging a facility fee for most telehealth visits and requiring disclosure of facility fees prior to a facility rendering services
Addressing Surprise Billing: Addressing ground or air ambulance transportation services rendered by an out-of-network provider for consumers and establishing arbitration and appeals procedure for disputes between providers and insurers.
Online Tools for Billing and Cost Transparency: Establishing online tools for consumers to identify cost-sharing or any out of pocket expenses associated with services and required disclosure of hospital service prices.
Most impactful, Georgia reformed its CON process as part of HB 1339. Under this bill, it removes a capital expenditure threshold for new health care projects or institutional health services that would be subject to review by the Georgia Department of Community Health, authorizes the Department to annually alter certain exemption criteria to CON standards for services and facilities, and exempts certain psychiatric or substance abuse inpatient programs from adhering to CON requirements, among other changes. In Connecticut, HB 5198 will prohibit telehealth providers from charging a facility fee for telehealth services through June 30, 2027. In Arizona, HB 2444 requires the development of arbitration procedures for out-of-network surprise billing disputes, with the intent to remove patients from the negotiation process. Finally, in Colorado, SB 24-080 was signed into law, which requires insurers to make an internet-based self-service tool available that provides real-time responses to consumer questions on cost-sharing information.
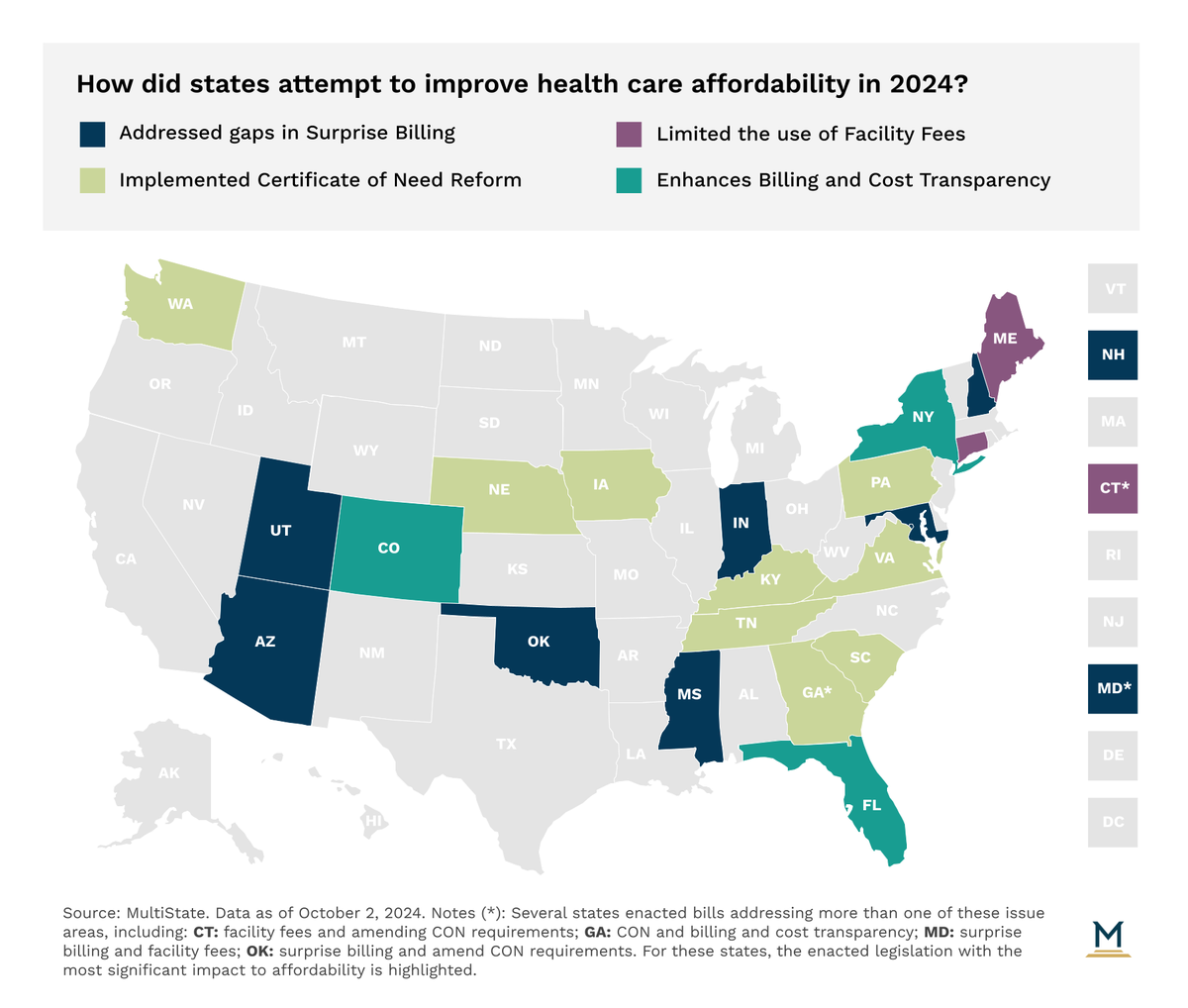
Despite the flurry of activity, a number of states are still attempting to find a unique solution. In 2024, legislation was introduced in 21 states to address surprise billing issues. Legislators in 12 states introduced bills prohibiting or limiting the use of facility fees. And policymakers in at least 25 states introduced legislation to reform CON standards, while lawmakers in 17 states introduced legislation to enhance billing and cost transparency for consumers.
We expect a similar flurry of activity this year. Given the complexity and depth of the health care supply chain, there is no single legislative solution. As a result, states will continue to utilize these policy levers to chip away at the cost. While red states may take action to incentivize enhanced competition between providers and increased access in efforts to reduce prices, blue states may be more likely to establish artificial cost controls based on cost growth assumptions. However states opt to implement their approach, these four provisions will continue to see the most attention in 2025.
The ever-evolving state health policy landscape will continue to influence how health care organizations make business decisions. MultiState’s team pulls from decades of expertise to help you effectively navigate and engage. MultiState’s team understands the issues, knows the key players and organizations, and we harness that expertise to help our clients effectively navigate and engage on their policy priorities. We offer customized strategic solutions to help you develop and execute a proactive multistate agenda focused on your company’s goals. Learn more about our Health Care Policy Practice.

December 18, 2025 | Brock Ingmire

December 15, 2025 | Mary Kate Barnauskas

November 5, 2025 | Mary Kate Barnauskas