
Technology & Privacy, Tax & Budgets, Health Care & Wellness
ICYMI: Major Emerging Legislative Trends in 2025 (Webinar Recap)
April 8, 2025 | Liz Malm
March 17, 2025 | Brock Ingmire

Key Takeaways:
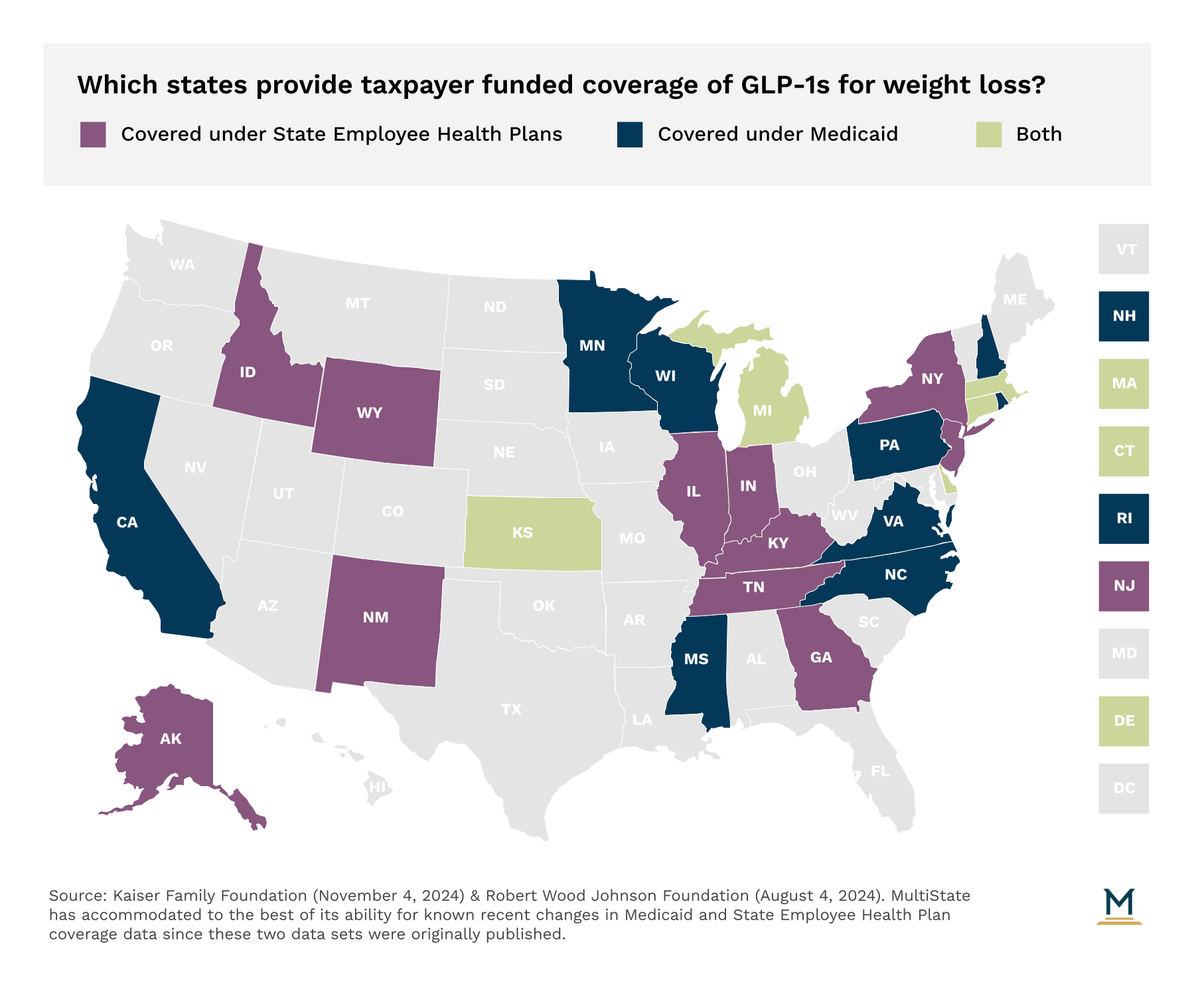
Despite some states offering limited coverage of GLP-1s to treat weight loss as far back as a decade ago, most states that currently provide coverage through taxpayer-funded Medicaid programs or state employee health plans have only opted to do so within the past five years. As of March 2025, 11 states cover GLP-1s for weight loss under their state employee health plan, nine states provide coverage under their state Medicaid program, and five states provide coverage under both programs.
Despite a significant number of bills in 2023 and 2024 that would have required mandated coverage of GLP-1s in Medicaid, state employee health plans, or for health insurers regulated by the state, only Arkansas, California, Maryland, New Mexico, Pennsylvania, and Texas have introduced legislation mandating coverage in 2025 to date. However, none of those bills are expected to gain traction this year.
In lieu of states expanding coverage, states that are committed to retaining coverage are looking at mechanisms to better control costs. Following Connecticut’s drastic increase in utilization under their state employee health plan, in 2023 the state began requiring enrollees to enroll in a telehealth program that sought to encourage full-scale lifestyle changes and eventually reduce dependence on GLP-1s and similar medications. Such efforts build from existing requirements, inclusive of in Michigan and Virginia.
One final consideration is that as more states establish upper payment limit (UPL) setting authority either for prescription drug affordability boards or other similar entities, it becomes increasingly possible that GLP-1s could be subject to review and UPLs across various states. If such were to happen, the door to expand access to coverage remains possible in the future.
Similar to Colorado, West Virginia and North Carolina have encountered similar cost challenges leading them to roll back their own coverage of GLP-1s for weight loss purposes from their state employee health plans. In West Virginia, the Public Employees Insurance Agency (PEIA) started a 1,000 person pilot program that covered GLP-1s to treat obesity beginning in 2019. PEIA opted to pause the program in 2024 citing a $1.3 million per month price tag, inclusive of rebates.
In North Carolina, the state employee health plan initiated coverage of GLP-1s for weight loss purposes in 2015. In January 2024, the state opted to pull back that coverage. The State Health Plan Board of Trustees concluded that coverage of these drugs for weight loss purposes was no longer financially feasible and would have required a premium increase of $48.50 per member per month. Following a 731 percent increase in utilization of the drug (up to more than 23,000 members utilizing GLP-1s for weight loss purposes) by 2024, the Board estimated the cost in 2024 to exceed $170 million and jump to more than $1 billion over the next six years.

April 8, 2025 | Liz Malm

April 2, 2025 | Townsend Brown

February 26, 2025 | Lisa Kimbrough