
Technology & Privacy, Tax & Budgets, Health Care & Wellness
ICYMI: Major Emerging Legislative Trends in 2025 (Webinar Recap)
April 8, 2025 | Liz Malm
December 17, 2024 | Brock Ingmire, Lisa Kimbrough, Mary Kate Barnauskas
-b4bc66-1200px.jpeg)
Key Takeaways:
In 2025, state lawmakers are expected to prioritize healthcare affordability and access, building on key legislative trends from this year. Here are our thoughts on key trends and issues from 2024 and how they might show up in state capitols next year.
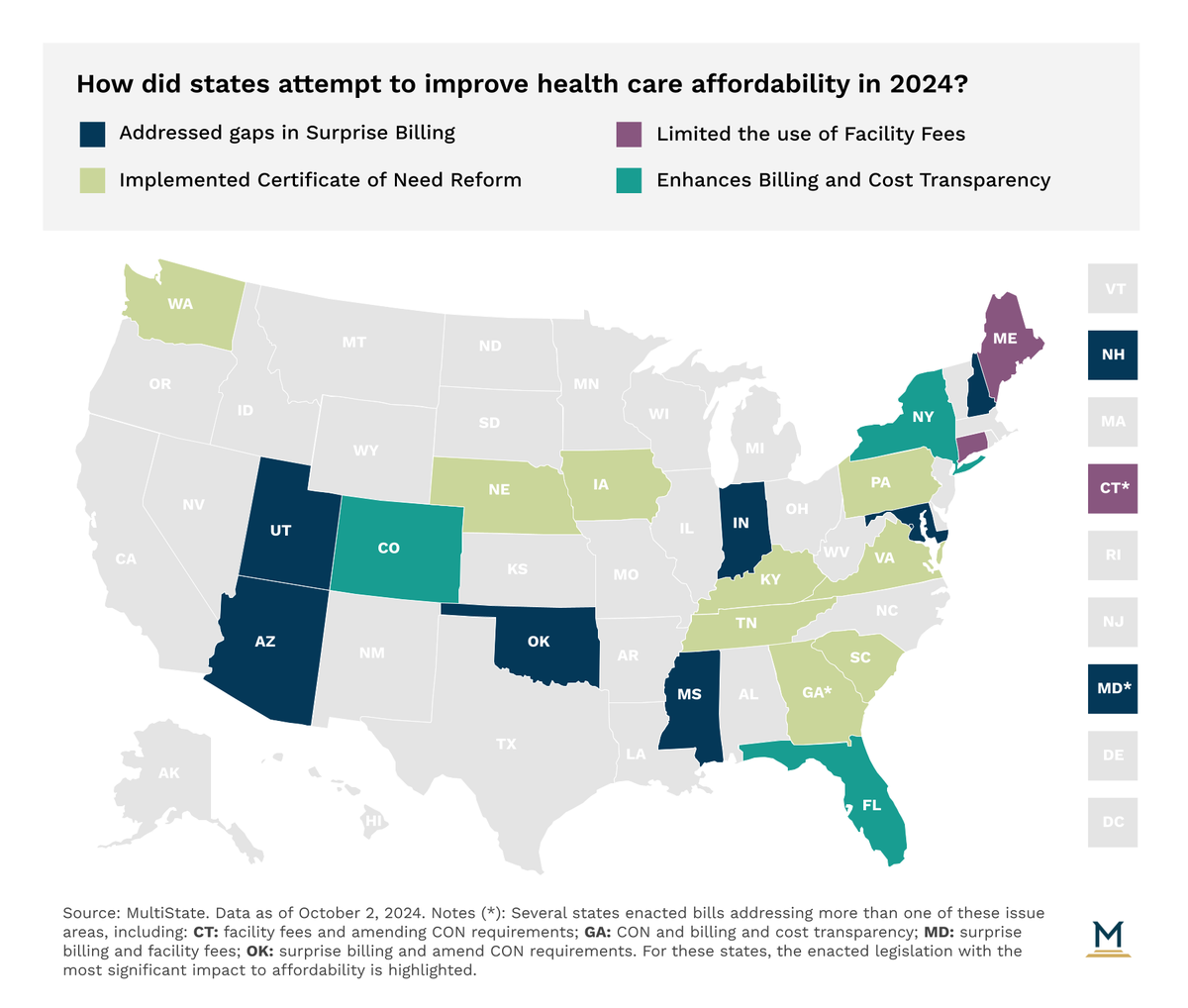
State lawmakers have taken note of rising healthcare costs. While prescription drug pricing has been a particular area of focus in recent years, lawmakers are now also looking at containing costs of provider services. Key legislative strategies on this front have included certificate of need reform, facility fee restrictions, surprise billing protections, and billing and cost transparency. In 2024, legislation was introduced in 21 states to address surprise billing issues. Legislators in 12 states introduced bills prohibiting or limiting the use of facility fees. And policymakers in at least 25 states introduced legislation to reform CON standards, while lawmakers in 17 states introduced legislation to enhance billing and cost transparency for consumers. We expect these areas to continue to be a priority for lawmakers in 2025, with red states looking to take action to incentivize competition between providers and increase access, while blue states may be more likely to establish cost controls based on cost growth assumptions.
Prescription drug pricing continues to see significant action in the states, with legislation addressing 340B growing in popularity. The 340B Program requires pharmaceutical manufacturers to sell outpatient drugs at a discount to qualifying providers with the intent of having qualifying providers spend the savings from the program to serve more patients and provide more comprehensive services in their communities. 2024 was a busy year for 340B legislation with 20 states introducing and 6 states (Kansas, Maryland, Minnesota, Mississippi, Missouri, and West Virginia) enacting legislation to prohibit or limit manufacturersʼ ability to not extend 340B pricing to contract pharmacies. We expect legislatures across the country to be active on this issue again in 2025, especially since courts in Louisiana and Arkansas upheld similar laws that were passed in 2023.
In 2024, 36 states considered and 18 states enacted legislation to limit prior authorization or require more transparency from insurers. Trends within prior authorization legislation include establishing “gold carding” models, which allows physicians with a proven track record of having specific procedures or treatments approved to be exempt from obtaining prior authorizations, and limiting prior authorization for certain conditions, such as cancer and mental illness. We expect these trends to continue in 2025, especially as gold carding is implemented in other states. In addition, lawmakers might take action to address prior authorization for popular semaglutide medications developed for the treatment of diabetes and now being used for weight loss.
The ever-evolving state health policy landscape will continue to influence how health care organizations make business decisions. MultiState’s team pulls from decades of expertise to help you effectively navigate and engage. MultiState’s team understands the issues, knows the key players and organizations, and we harness that expertise to help our clients effectively navigate and engage on their policy priorities. We offer customized strategic solutions to help you develop and execute a proactive multistate agenda focused on your company’s goals. Learn more about our HealthCare Policy Practice.

April 8, 2025 | Liz Malm

April 2, 2025 | Townsend Brown

March 17, 2025 | Brock Ingmire