
Technology & Privacy, Tax & Budgets, Health Care & Wellness
ICYMI: Major Emerging Legislative Trends in 2025 (Webinar Recap)
April 8, 2025 | Liz Malm
January 6, 2025 | Lisa Kimbrough

Key Takeaways:
During the 2024 state legislative sessions, 33 bills were enacted in 20 states related to the regulation of pharmacy benefit managers (PBMs). Most of the enacted legislation focuses on spread pricing, 340B pharmacies, patient steering/affiliated pharmacies, and increased reporting of PBM activities.
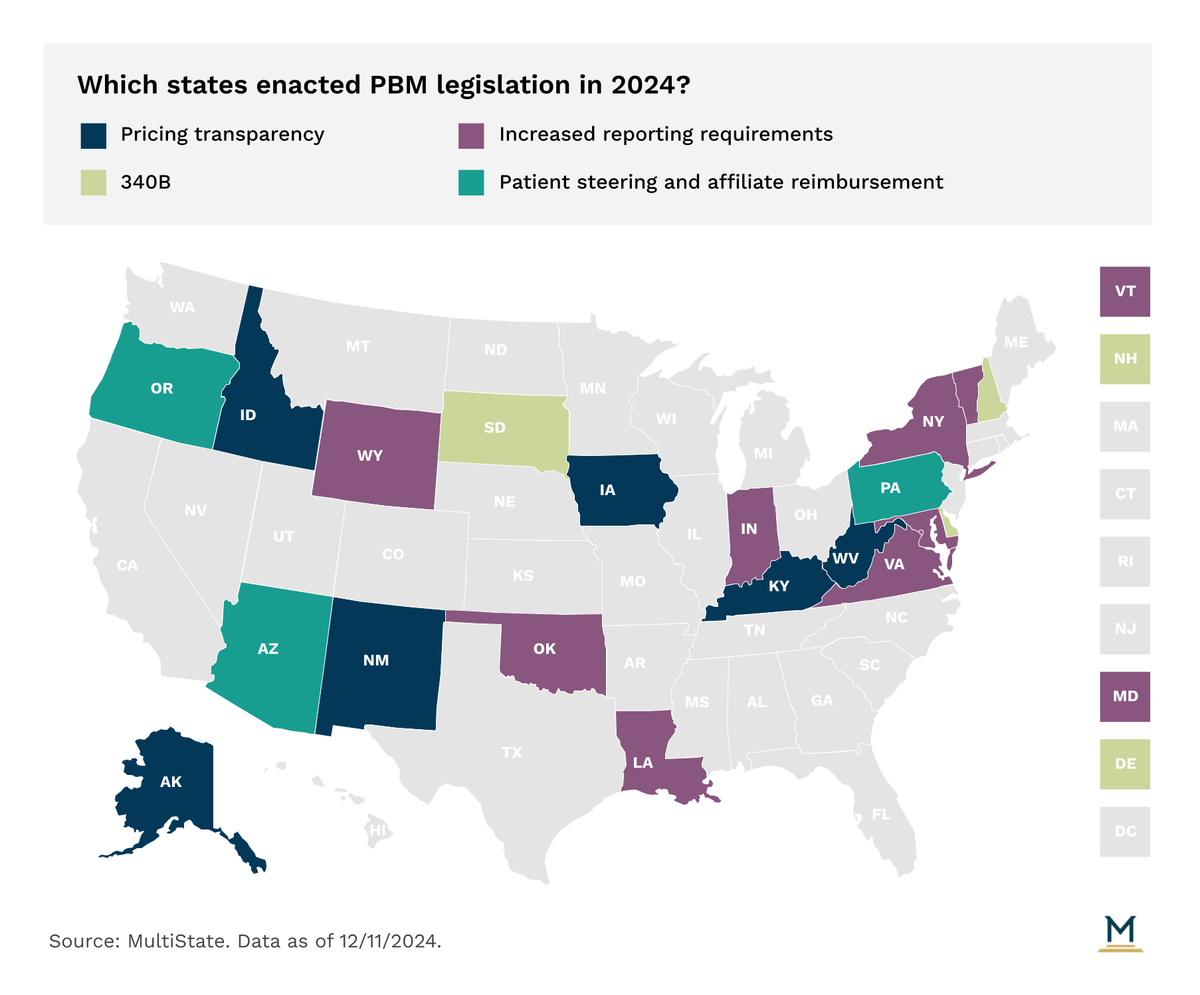
In the increasingly diverse methods states are using to get a handle on drug pricing, one that has been proposed in a number of states and enacted in 16 is a prohibition on spread pricing. Spread pricing is when PBMs charge a health plan for a drug a different amount than that paid to the pharmacy for filling the prescription. This is sometimes done when PBMs charge less for expensive, infrequently prescribed drugs, but more for cheaper, more widely used drugs. Sometimes PBMs simply overcharge for all drugs. In 2024, Idaho and Vermont enacted laws prohibiting spread pricing. Prohibiting spread pricing reduces costs and makes spending on drugs more predictable, which is beneficial to state employee health plans and Medicaid programs that rely on state budgets. Audits done in the District of Columbia and Pennsylvania in the last couple of years showed that Medicaid programs were overcharged by average of $5 million to $7 million annually due to spread pricing.
As we’ve previously noted, the 340B program has been in 2024 and will continue to be in 2025, a focus of state legislative action. The focus of legislation regarding PBM interaction with 340B contract pharmacies will be to limit discriminatory behavior on the part of PBMs. Delaware, New Hampshire, and South Dakota each enacted bills ending discrimination against 340B contract pharmacies by PBMs. In all three bills, “discrimination” includes reduced reimbursement rates as compared to non-contract pharmacies, increased fees as compared to non-contract pharmacies, and additional conditions as compared to non-contract pharmacies. The South Dakota bill goes further, allowing 340B entities to bring civil action against PBMs for any discriminatory behavior.
Patient steering bills usually manifest as prohibitions on PBMs mandating that patients only obtain prescriptions from affiliated pharmacies or mail-order pharmacies owned by the PBM. By 2022, 18 states had adopted anti-steering legislation, but in 2023 no new states added it to their arsenal of PBM reforms. This year, only Pennsylvania enacted legislation banning patient steering. Two states, Arizona and Oregon, went in a similar but slightly different path. Those states prohibit PBMs from reimbursing affiliate pharmacies more than non-affiliated pharmacies. Thus, removing some of the incentive for patient steering.
Finally, some states extended reporting mandates on PBMs. Specifically, New Hampshire, New Mexico, and Virginia all require PBMs to report the rebates they receive from manufacturers. Louisiana has taken this another step further and requires rebates to be passed through to the insurer. This is a track more states are expected to take in 2025.
The ever-evolving state health policy landscape will continue to influence how health care organizations make business decisions. MultiState’s team pulls from decades of expertise to help you effectively navigate and engage. MultiState’s team understands the issues, knows the key players and organizations, and we harness that expertise to help our clients effectively navigate and engage on their policy priorities. We offer customized strategic solutions to help you develop and execute a proactive multistate agenda focused on your company’s goals. Learn more about our HealthCare Policy Practice.

April 8, 2025 | Liz Malm

April 2, 2025 | Townsend Brown

March 17, 2025 | Brock Ingmire